Recently, my body has been treating me to some different symptoms than I’m used to. Some are blasts from the past, others are brand new. Both have left me feeling more acutely unwell. My GP is on maternity leave so while I navigate these new bodily (mal)functions, I’ve been getting to know a couple of new doctors, or rather they’ve been getting to know me, in alarming detail…
Meeting a new doctor always brings up some sore feelings for me and involves going through the motions of doubt even the most well-meaning doctors seem to have, especially, but not limited to, believing women’s testimonies of pain. Once I got the endometriosis diagnosis confirmed, I remember thinking that although it was bad news, at least now doctors would have to believe me. Yet the last three times I’ve told a doctor that I have endometriosis, it has been met with scepticism. ‘So why do you think you have endometriosis?’, ‘we can’t know that for certain without surgery,’ ‘and has that been confirmed by laparoscopy?’ are the responses I’ve received. Perhaps I’m paranoid and I’m as suspicious of them as they are of me, but it immediately makes me cringe, knowing that what they’re really asking is: ‘is that a self-diagnosis?’ It stings all the more after I deliberately made a point of never saying ‘I have endometriosis’ before a surgeon found it – hell, didn’t I call it dementors? Another side to this is the uncomfortable truth that actually, I did think it was endometriosis, I did self-diagnose and I was right, it just took three and a half years and two surgeries for a doctor to concur.
At one of these appointments the doctor wanted to perform a pelvic exam. I asked if there was a way I could do what needed to be done myself and when she said no, I explained my hesitation around pelvic exams, the associated pain and my pelvic floor dysfunction. Minutes later, when I’m crying in pain and she can’t find my cervix, the doctor looked up between my legs in panic and said, ‘oh god, is it like this for you every time? I’ll try to be quick!’ She was visibly quite shocked and suddenly started asking more questions and taking me seriously. I just sat there thinking about how the examination didn’t need to be like that, if only you’d listened to, believed and processed what I said before it. Why else would I have said it? I would love to know the answer to this question because I reckon it’s steeped in unconscious biases. Doctor friends, enlighten me! Let’s fix this!
Back to the present day, I’ve still got eight months until my appointment with my new gynaecologist, the first endometriosis specialist I’ll have ever seen. I’m also a month away from a colonoscopy. After months of recurrent rectal bleeding I had a slightly more serious ‘episode’ (it was actually hours after the aforementioned pelvic exam). Apparently I should have taken myself to A&E, instead I went home, freaked out and went to sleep. I’m now in a sense of heightened anxiety about going to the loo, because if there is a repeat of this episode, then I’m under strict instructions to take myself straight to hospital. My GP went through the possible outcomes of the colonoscopy, many of which are a little scary, before ending rather perkily with the alternative outcome: ‘it’s probably just the endometriosis!’
While I’m patiently waiting for this mystery to be solved or at least identified, of course my body decided to help me along by giving me a UTI followed by the familiar feeling of kidney pain, sending me to the out of hours doctor on a Saturday night with a suspected kidney infection. The doctor concluded it was either the beginning of a kidney infection or the end of a serious UTI and to keep an eye on it, and then, just as I was leaving the consultation room, she added, ‘it’s also probable it’s just the endo. It can cause a lot of pain, you know.’
I’ve heard that logic twice in two weeks. ‘It’s probably just the endo!’ Is it supposed to reassure me? I don’t want it to be the endo. I don’t want to have to deal with the fact that endometriosis has taken over my bowels and urinary system as well as my sexual and reproductive organs, mostly because, in all likelihood, no one will know what to do with that information. At least we know how to treat kidney infections. Saying, ‘it’s probably just the endo,’ however true it might be, is not particularly helpful or likely to result in relief any time soon.
The doctor I will see later this year recently appeared on a Flemish documentary about endometriosis and I was very happy to hear her say that she works together with gastroenterologists and urologists, knowing that more than one expertise is needed to deal with endometriosis. This gives me a lot of hope in the case that these unexpected symptoms are ‘just the endo.’ I just hope my body can cool the drama until then. In the meantime, the colonoscopy will take place in French and my new gynaecologist is in Flanders, so I have some vocab to swot up on…
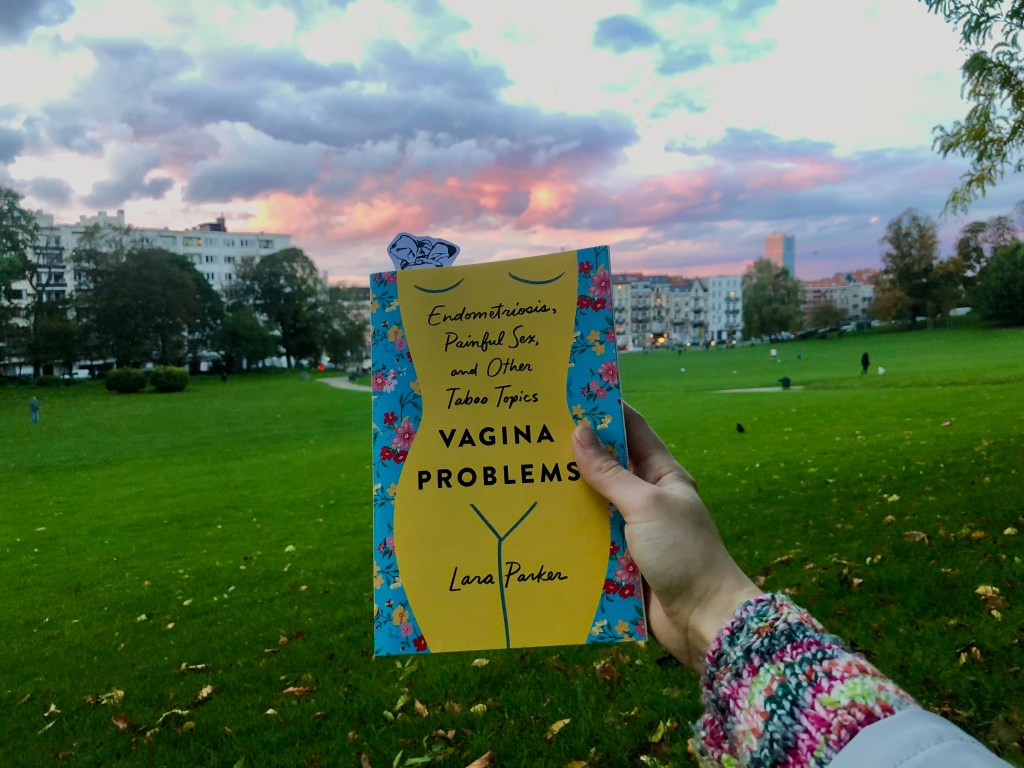
Next month is endometriosis awareness month! Endometriosis UK are running an #EndoTheStigma campaign and are running lots of great online events including this one on Endometriosis and Sex during COVID-19, get involved!
Also, did you hear? The Birthrights charity is convening a national inquiry into racial injustice in maternity care. This is a long time coming, follow its progress here.