I spent much of the last blog complaining that one problem with endometriosis is that eyeing it up as a suspect for any new or re-emerging symptom is unhelpful because treatment = surgery and waiting times = incredibly long, especially at the moment. Shortly after I wrote that, the universe said ‘hold my beer.’ The pace has picked up. Significantly. That gynaecologist appointment I had scheduled for September, the one I’ve been on the waiting list for since last September? Well, that’s now been rescheduled for April. (April 2021 – I checked). Why the sudden change of plans? Because the colonoscopy revealed, as much as I don’t want to hear it, that actually, it is the endo.
Let’s step back a second. I went into the colonoscopy highly stressed. I was already anxious about it, in part because in Belgium colonoscopies are performed under general anaesthetic as standard and I’m currently separated from my family by a pandemic and a new political border. This meant I had to turn to my wonderful friends in Brussels to chaperone me home from the procedure. But then of course, the day before the procedure everything that could have gone wrong went wrong. From the first set of laxatives making me pass out, to my neighbour’s radiator leaking into my flat and my dear friend and chaperone getting covid. It all culminated in one very strange and stressful afternoon of me sitting at my desk, trying to work, sipping laxatives, lining up another angelic friend to escort me home from hospital while two men smashed a hole through the ceiling.
By the time it came to the procedure, I was suddenly grateful I’d be under general anaesthetic, a chance to sleep – at last! A good thing about the stressful build-up was that I didn’t have time to dwell on the outcomes of the colonoscopy, although I will say I had rather cynically decided that it was yet another unnecessary and invasive procedure that would more than likely result in absolutely nothing. This was also along the same lines as the last thing the gastroenterologist said to me before I went under.
When I came round, not only was I thrilled to find that my anus still felt relatively normal but I was greeted by a surprised and slightly confused gastroenterologist. She had found something after all – a lone ulcer in my colon. She said it was strange. If it were Crohn’s or Ulcerative Colitis, then there would be more than one ulcer. She said it could be that we’d found one of the two inflammatory bowel diseases very early on, but that it seemed unlikely. Either way, it was a serious answer to why I have been experiencing rectal bleeding. She handed me a letter to give to my GP, with some options to explore.
It’s fair to say that I’ve been miserable company since then – it’s a good job I live on my own at the moment. My GP took the reins and has been brilliant, communicative and actively exploring scientific papers and new hypotheses with me. But the day after the procedure she rang me to inform me that whatever happens now, I cannot take ibuprofen. It’s hard to describe how significant this is without sounding completely OTT. For the last five years, pre and post diagnosis, through every treatment I’ve tried, ibuprofen has been the only reliable pain relief I have had that doesn’t send me to sleep, mess with my head, make me lactate (yes, really) and that actually reduces the pain enough for me to enjoy myself or concentrate for a few hours. To be told that the solutions to new and old problems are still unknown while having my main crutch taken away… it’s really tough.
Tough even more so because as much of my social bubble gets excited about the potential end of lockdown life in the UK, I’ve already been feeling nervous about a return to normality. Working from home has been much easier for pain management, the idea of working in the office without ibuprofen is terrifying because I know I can’t do it. Things in Belgium are very different from the UK though, and a return to ‘normality’ is further out of reach. My GP is taking my concerns about pain management seriously though and promises that we’ll have a new plan by the time office life, all-day weddings and adventures begin again.
We (my GP and I – a team, at last! This is how it should be!) both did a lot of work to follow up on the colonoscopy. My doctor chased the biopsy results and asked them to test for endometriosis if they could. They weren’t able to unfortunately but they have, thankfully, ruled out Chron’s and colitis. This means with some certainty that the ulcer in my colon is caused by endometriosis: either a secondary cause in that the ulcer was caused by too much ibuprofen or a primary cause, meaning that it might not be an ulcer at all, but an endometriosis lesion. Both these theories are backed up by the fact the rectal bleeding tends to happen the day after an uptick in ‘period’ pain. My job was to let my new gynaecologist’s office know of the news and our concerns around it, hoping that it might lead to a bump up the appointment list. And it did!
This is good news because it’s a step forward, rather than just standing still as I’ve been for the last 18 months. However, it could mean that more surgery is on the horizon sooner than I expected and I do not relish that thought.
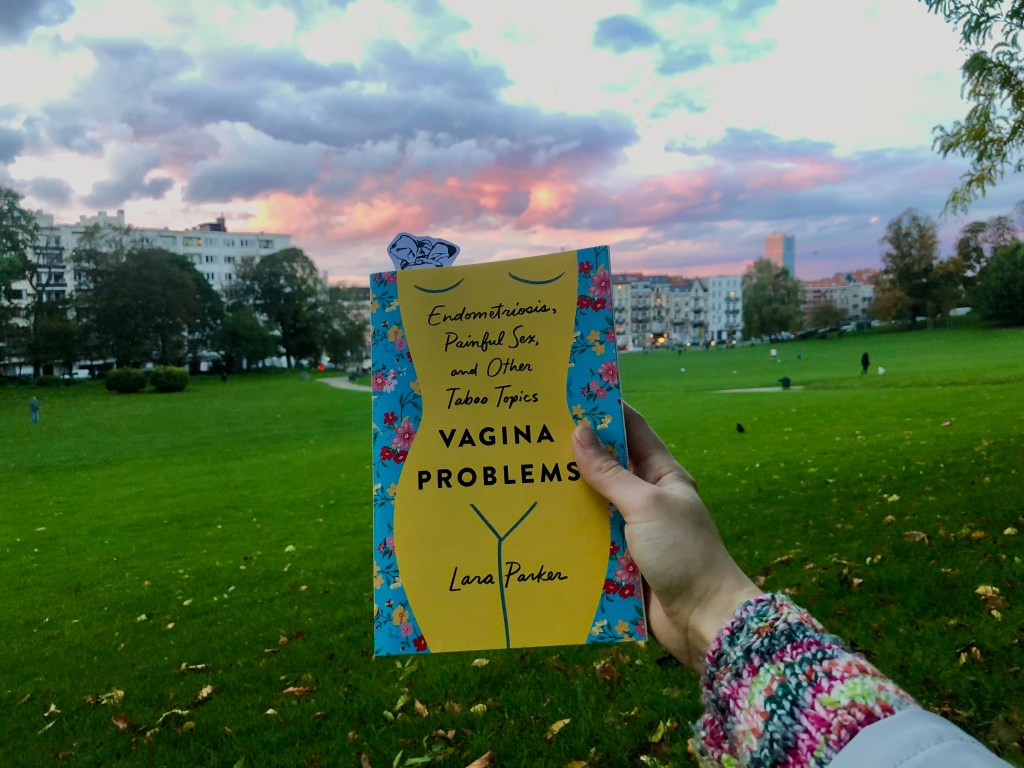
I’ve found this month so far, which is also Endometriosis Awareness Month, difficult and emotional. When I found out about the ulcer, I realised I’d been doing it again, telling myself that I’d imagined the symptoms. I understand why I’ve developed this behaviour but the come down from realising that something is wrong and that I did the right thing by asking for help is still quite a shock to the system. The day after the colonoscopy I joined the Vaginismus Network’s meeting. I always find these meetings moving but Sarah Rose McCann, whose own experience is not dissimilar to my own, spoke and had me sobbing. It was super cathartic and her talk and the whole event was incredibly inspiring, but I was just overwhelmed with some kind of grief. I was really, really sad that so many of us are still in so much pain, still searching for answers, still not being taken seriously, and now, it seems, I’m not even taking myself seriously. I hope my blog is part of the collective action that will raise awareness of and soon see the back of so much suffering.
The British government is running a consultation on the future women’s health strategy for England. Like many, I’m deeply sceptical and am still waiting to see policy changes and, more importantly, improved health outcomes. Yet if we don’t complete the consultation then our voices will go unheard. So I will be completing the consultation and I hope you will too. It’s also important as many voices as possible are represented in the consultation, and if it’s just a bunch straight, white women like myself taking part then it will be about as useful as a chocolate teapot. So share it with all the womxn you know, let’s give the government more than they bargained for and demand change.